Most patients and families want the ability to communicate with care providers the same way they communicate with friends and family: electronically. They want to be able to ask health questions, schedule appointments and share new health concerns online. Care teams also benefit—in a 2019 study, physicians said online messages help them build better relationships with patients. Electronic messaging also increases patient access without burdening the phone lines and improves efficiency by allowing asynchronous communication any time of day.
However, these benefits come with a cost. They require providers to spend substantial time responding to the messages, which adds stress, contributes to burnout and interferes with face-to-face patient care, according to a study by the American Medical Association.
At Cleveland Clinic’s Children’s Hospital, pediatric providers and clinical staff said they felt overwhelmed by patient portal messages and had trouble responding in a timely manner. Using EHR data, the hospital found that 20% of patient messages in 2018 did not receive a response or the response took longer than three business days, which is the hospital’s standard.
Concerned that this contributed to unsatisfactory patient experiences and clinician burnout, Cleveland Clinic Children’s initiated a quality improvement project with a multidisciplinary team to evaluate the process of portal messaging. The project led to changes that ultimately reduced staff burnout, improved response times and increased staff satisfaction—all of which led to better patient care.
Identifying the problems
The first step was to understand the current process for responding to patient messages and identify pitfalls. The project team started by interviewing multiple stakeholders—including medical assistants, nurses and clinicians—about their attitudes and experiences with patient portal messages and asking them to identify barriers and solutions based on their experience.
Then the team mapped the current process. Each member of the diverse team—a quality improvement coach, triage nurse, medical assistant, pediatrician and nurse who manages the EHR software—provided perspectives on the workflow and revealed several mistakes at each step:
- Message arrives in the medical assistant pool. At this step, medical assistants were trying to answer the message but did not have the clinical knowledge to do so. Or the message was routed to the wrong place (for example, to the physician when it should have gone to the nurse). Sometimes, for various reasons, the message was not routed at all.
- Message goes to nurse triage pool. Nurses were double-charting because they had to call the patient and then route both the phone call and the message to the physician.
- Message goes to provider. The message was overlooked among the other messages in the provider’s inbox
To understand whether these findings resonated with other clinicians and staff, and to identify additional areas for improvement, the team created a short survey. The baseline survey was sent to all pediatric providers and used Likert scales to evaluate their experiences with the portal messaging system. The survey included questions on their level of knowledge using the system, satisfaction with the current workflow, ease of responding to a message, confidence in responding to or routing a message, and frustration with their workflow when replying to messages. Additionally, the survey asked about their level of burnout and their urgency to respond to messages.
From the survey results, interviews and process map, the team found that most caregivers had unclear routing instructions, used non-standardized messaging, missed urgent messages, and lacked time to complete them on top of a busy workday.
Developing solutions
With this data in hand, the team convened an educational session with pediatric providers to outline solutions. During the session, the project team clarified the workflow and provided clear instructions on when a message should be triaged, using specific examples.
The team also introduced standardized responses, called smart phrases, for several different scenarios—requests for prescription refills, billing information and appointments, and messages routed to the provider or the nurse. For example, nurse triage messages always use the smart phrase, “Thank you for your request. Your message has been forwarded to Nurse Triage who will be contacting you by phone so we can better understand your concern.”
These smart phrases ensured consistent responses no matter who answered the message or what the request was. The team also placed a reminder card at each workstation displaying instructions for the smart phrases based on the patient’s message. After the educational session, medical assistants were able to identify which messages they could reply to with smart phrases and which should be escalated to the nurse triage pool or the provider inbox.
The team also added a feature to the system that automatically returns messages to the pool if they have not been routed within a certain time frame, ensuring messages no longer go unanswered.
Long-term results
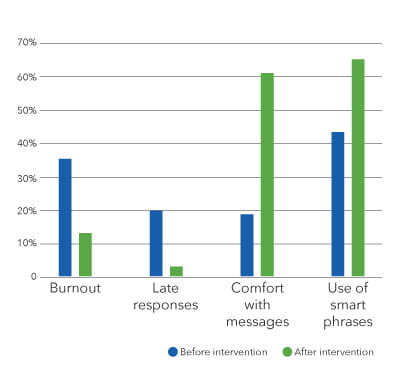
Eight weeks later, the team sent out the survey again to evaluate the effectiveness of the interventions. Sixty percent of staff surveyed responded. When the team compared pre-results to post-results, they found less burnout with messages, higher use of smart phrases, and increased comfort in responding to messages.
To evaluate the sustainability of the new workflow, the team used EHR data to measure the time to respond to messages six months after changes were implemented. They found that the percentage of messages without a timely response decreased from 20% to 2.5%.
In the open-ended section of the post-survey, many respondents commented on the consistency and ease of the new process. One shared, “This was exactly what needed to be done, and it assured successful use by staff. This was a painless way to obtain staff buy-in, and now we love it.”






