The procedure itself is not new. As Jonathan Cheng points out, nerve transfer surgeries—in some form—have been performed for nearly two decades. But evolving technology is making the process an increasingly viable solution for patients with acute flaccid myelitis (AFM).
"The options have expanded due to a number of innovations and our understanding of the internal anatomy, the organization of the nerves and how the human body is able to control those nerves," says Cheng, M.D., pediatric hand and peripheral nerve surgeon at Children's Health in Dallas, and associate professor of plastic surgery at the University of Texas Southwestern Medical Center. "It's a surgical strategy that has really created a revolution in the reconstruction of severe nerve injuries."
Acute flaccid myelitis (AFM) presents challenges
While it's still very rare—the CDC estimates that fewer than one to two of every 1 million children in the United States will get AFM annually—the number of cases has risen steadily in the past five years. Young children are most susceptible and generally experience weakness in their extremities and sometimes paralysis.
With the help of medications and physical therapy, patients may regain some limb movement. Nerve transfer surgery is an option, but AFM's characteristics present challenges:
- Where to operate. Because some muscles will regain mobility without surgical intervention, determining if—and on what nerves—a transfer surgery is necessary is difficult. "When a nerve is initially injured, even if it's going to recover on its own eventually that may not necessarily be apparent," Cheng says. "By far, the most difficult part of the decision-making process is to leave things alone that are going to heal on their own, to fix the things that are not going to heal on their own and to be able to tell the difference."
- Timing. Muscles typically must regain nerve supply within 18 months to restore function, so Cheng says the optimal timing for nerve transfer surgery would be nine to 12 months from AFM onset. Reliable electromyography (EMG) testing helps the care team make critical decisions within this timeframe, according to Cheng.
- Post-operation. It can take nine to 12 months to know if the surgery was successful. Cheng says precise recordkeeping is critical to analyze the procedure later, and it's important the patient and family are aware of the time required for post-surgery recovery and rehabilitation.
Time is of the essence
Because there's a relatively short window of time for a nerve transfer surgery to successfully treat AFM, early diagnosis and treatment is critical. "We have to see them early enough, which is where the importance of both patient and physician education come into play," Cheng says. "Just as it's really important for the hospital and emergency care teams that initially encounter the patient to recognize the onset of AFM to know what they may be looking at and how to intervene."
A strong team effort is also crucial to success. "It's important to emphasize the multi-disciplinary nature of this," Cheng says. "It's critical for these patients to have experienced neurologists looking after them and to have all the different folks with their different expertise on board to look after their overall needs before embarking on these types of (nerve) reconstructions."
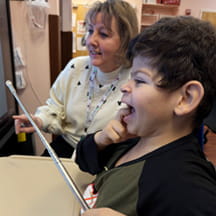
Impact of surgery is "immeasurable"
For AFM patients and their families, the effects of AFM are sudden and often devastating. Through nerve transfer surgery, Cheng and his colleagues—in the face of the disease's uncertainty and challenges—can profoundly influence the lives of these patients. "It has a tremendous impact on their quality of life," Cheng says. "In some ways, those impacts are immeasurable."